PATIENT SPECIFIC (PSI), KINEMATICALLY ALIGNED TOTAL KNEE REPLACEMENT
Advanced planning meets personalised alignment for a more natural-feeling knee replacement
PSI | KA | TKA
Total knee replacement surgery is a procedure designed to relieve pain and restore mobility in patients with severe knee arthritis or joint damage. The surgery involves removing the damaged parts of the knee and replacing them with a prosthetic joint, which is carefully designed to replicate the function of a healthy knee. Traditionally, implants have been positioned using standardised techniques that apply the same alignment principles to every patient however, not all knees are the same and newer approaches now focus on tailoring the procedure to each individual.
If you are considering total knee replacement surgery, you may benefit from an approach that is both patient-specific and kinematically aligned. This combination of surgical precision and personalised alignment aims to restore the natural movement of your knee while supporting long-term function and comfort.
In the sections below, you’ll learn more about how patient-specific, kinematically aligned knee replacement works, and whether this highly personalised surgical option may be right for you.

What is a patient-specific (PSI) total knee replacement?
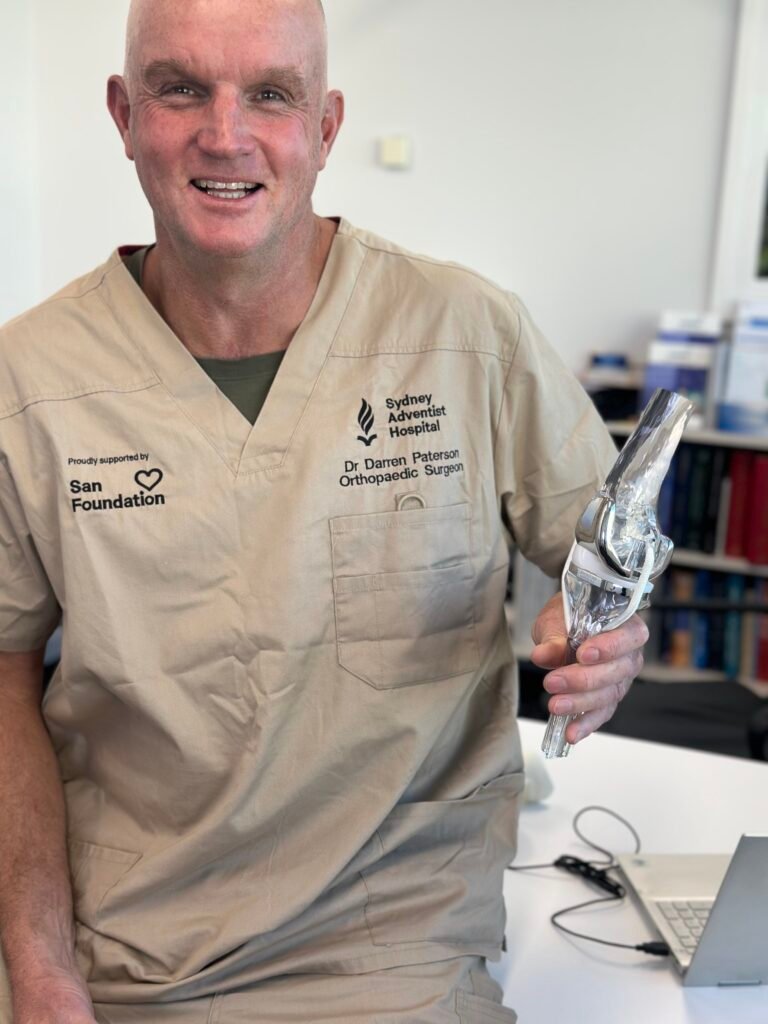
Patient-Specific Instrumentation (PSI) is a surgical planning and execution technique that uses your own MRI or CT scans to create customised 3D models of your knee. From this detailed imaging, precise surgical guides are created to match the shape and alignment of your joint. These custom guides assist Dr Paterson in making highly accurate bone cuts and positioning the prosthetic components in alignment with your natural knee anatomy. This can be particularly beneficial when combined with the kinematic alignment technique, which aims to preserve your joint’s natural motion patterns.
Understanding kinematic alignment
Kinematic alignment is a modern and highly individualised technique used in total knee replacement surgery. Unlike the traditional mechanical alignment method which, positions the implant along a straight axis from the hip to the ankle, kinematic alignment aims to restore your knee’s original, pre-arthritic alignment and movement patterns.
This means that instead of forcing every knee into the same alignment, the surgery is tailored to match the natural angles, shapes, and motion pathways that were present before arthritis developed. The goal is to recreate a knee that moves and feels more like your own.
By closely preserving the natural orientation of your ligaments, joint lines, and bone contours, kinematic alignment offers the potential for:
- More natural knee motion that aligns with how your body moves
- Reduced soft tissue trauma, since the ligaments and muscles don’t need to be artificially tensioned or rebalanced
- Improved comfort and stability during walking, climbing stairs, and other daily activities
- Faster return to movement, especially when combined with personalised instrumentation and early rehabilitation
There are two key surgical techniques used to achieve kinematic alignment during total knee replacement. Both are designed to restore your natural joint movement by accurately replicating your knee’s pre-arthritic anatomy. Dr Paterson is experienced in both methods, with a strong preference for the Patient-Specific Instrumentation (PSI) technique for its high level of accuracy and individualisation.
This method involves advanced 3D imaging, using either an MRI or CT scan, to create customised, patient-specific cutting guides tailored to your unique knee anatomy. These 3D-printed guides help position the implant with exceptional precision, aiming to restore your natural joint line, alignment, and motion patterns.
This approach supports:
- Minimal soft tissue disruption
- Accurate bone cuts matched to your original knee structure
- A smoother, more natural-feeling joint post-surgery
PSI reflects Dr Paterson’s commitment to combining leading-edge technology with a patient-centred approach.
This method uses manual measurement tools (callipers) during surgery to recreate your natural joint geometry. It relies on careful intra-operative assessment to ensure accurate replication of bone thickness, joint angles, and limb alignment.
While effective, this technique does not benefit from the same degree of preoperative customisation as PSI so, by prioritising PSI-guided kinematic alignment, Dr Paterson delivers a personalised and precise total knee replacement that may offer improved comfort, range of motion, and overall joint satisfaction following surgery.
This approach respects the individuality of each knee, recognising that no two joints are exactly the same, even within the same person.
Potential benefits of combining PSI and kinematic alignment
Combining Patient-Specific Instrumentation (PSI) with kinematic alignment brings together two advanced techniques that allow your total knee replacement to be tailored specifically to your unique anatomy. This combination offers several potential benefits for comfort, function, and recovery.
PSI uses detailed imaging (MRI or CT scans) to generate custom-made surgical guides that match your individual bone structure. When paired with the kinematic alignment approach, which restores your knee to its natural, pre-arthritic alignment. This ensures the implant is placed in a position that closely replicates how your knee used to move.
This level of precision aims to:
- Restore your natural joint line
- Respect the existing soft tissue balance
- Reduce the need for ligament releases or muscle disruption during surgery
Traditional mechanical alignment places the implant in a generic, straight position. By contrast, combining PSI and kinematic alignment allows the implant to follow your original joint orientation.
This may help the new knee feel more like your own, improving:
- Comfort during daily activities
- Confidence when walking or bending
- Satisfaction with how the knee performs during low-impact activities
PSI provides a detailed surgical plan well before entering the operating theatre. This can improve the accuracy of each bone cut and component placement, which is critical for long-term implant function and reducing the risk of complications.
Combined with the principles of kinematic alignment, this precision may:
- Minimise implant malalignment
- Reduce the risk of early wear or loosening
- Support long-term durability of the knee replacement
Because this approach often requires less disruption to surrounding soft tissue and results in a more natural alignment, patients may experience:
- Less post-operative discomfort
- Faster return to walking and rehabilitation exercises
- Smoother transition back to regular daily activities
When your knee replacement matches your original biomechanics, there may be less stress placed on the surrounding ligaments and soft tissues. This can help maintain joint balance and stability over time, potentially supporting a longer-lasting result.
Dr Paterson favours the combination of PSI and kinematic alignment because it allows him to deliver a highly individualised surgical approach that aims to improve patient comfort, movement, and satisfaction after total knee replacement. During your consultation, he will review your imaging, discuss your options, and explain whether this tailored method is suitable for your specific condition.
How Dr Paterson plans your total knee replacement procedure
Dr Paterson uses advanced MyKnee planning software to digitally reconstruct your knee and simulate the surgery before it happens. This software:
- Converts MRI or CT data into 3D anatomical models
- Designs PSI cutting guides tailored to your joint
- Supports preoperative planning for kinematic alignment
- Enhances precision during surgery by guiding bone resections and implant placement
This preoperative customisation allows Dr Paterson to visualise and plan every step of your operation, helping reduce variability and optimise your outcomes.
Your patient specific, kinematically aligned total knee replacement journey with Dr Darren Paterson: step by step
Undergoing a total knee replacement is a significant decision, and understanding the process can help you feel more confident and prepared. Dr Darren Paterson uses a highly personalised approach that combines Patient-Specific Instrumentation (PSI) and kinematic alignment, supported by the minimally invasive subvastus approach, to help restore your natural joint movement and improve long-term comfort. Here’s what you can expect from start to finish:
Your journey begins with a referral from your GP and an initial consultation with Dr Paterson. He will assess your knee’s alignment, stability, range of motion, and how your symptoms impact your everyday life. You’ll discuss whether total knee replacement is the most suitable option for your condition and what outcomes you can expect from surgery.
Once a decision is made to proceed, Dr Paterson will arrange for a CT scan of your entire leg. This scan provides detailed information about your bone structure and joint alignment, which is used to build a 3D model of your knee. This model forms the foundation of your customised surgical plan.
Using specialised planning software, Dr Paterson creates a precise surgical plan that maps out your implant positioning, sizing, and alignment based on your unique knee anatomy. This behind-the-scenes step typically takes 2–3 weeks and helps ensure the procedure is tailored to match your natural joint structure as closely as possible.
Before surgery, you’ll be provided with detailed instructions. This includes:
- Completing hospital admission paperwork
- Starting prehabilitation physiotherapy
- Booking your post-operative review appointments
- Preparing your home environment for recovery
Dr Paterson’s team will support you through each of these steps.
You’ll receive a pre-operative consultation with the anaesthesia team, usually by phone. Together, you’ll decide whether general anaesthesia or spinal anaesthesia is best for you, based on your medical history and preferences.
Before surgery, Dr Paterson will review the procedure with you, including the risks, benefits, and expected recovery. Once you’re confident and informed, you’ll sign a consent form. You’ll also receive advice on preparing your home and organising any support you may need after surgery.
Your 3D-printed cutting guides are manufactured in Switzerland, sterilised, and delivered to the hospital in time for your procedure. These instruments are uniquely designed to match your knee, ensuring the most accurate fit possible.
You’ll be admitted to hospital on the day of your surgery, usually a few hours before the scheduled procedure. The nursing and surgical team will prepare you and confirm that all pre-operative protocols are in place to ensure a smooth and safe operation.
Fasting Instructions
Your anaesthetist or hospital will provide specific instructions about fasting (not eating or drinking) before surgery. In most cases, you will be asked to:
- Stop eating at least 6 hours before your admission time
- Stop drinking clear fluids (e.g., water) 2 hours before surgery
It’s important to follow these instructions carefully to ensure your safety under anaesthesia. If you’re unsure about the timing, check with the hospital the day before.
What to Bring to Hospital
To help you feel comfortable and prepared, we recommend packing the following:
- Your hospital admission paperwork
- Any current medications in their original packaging
- Comfortable loose-fitting clothing for after surgery
- Slip-on shoes or supportive footwear (no laces)
- A list of any known allergies or medical conditions
- Personal items such as glasses, hearing aids, or dentures (if applicable)
- Your Medicare and private health insurance cards
- Mobile phone and charger (if desired)
Leave valuables and jewellery at home and remove any nail polish from your fingers and toes prior to arrival.
A nurse will help you change into your surgical gown and complete final checks. Once ready, you will be escorted to the operating theatre when it’s time for your procedure.
The surgical procedure
In the anaesthetic bay, you’ll meet your anaesthetist and receive your agreed anaesthetic. Once you are comfortable and asleep or sedated, your leg will be cleaned with antiseptic solution and sterile drapes will be placed around the knee. A tourniquet may be applied around your thigh to reduce bleeding and improve visibility during the procedure.
Dr Paterson will make a careful incision along the front of your knee. He uses the subvastus approach, a minimally invasive technique that gently lifts (rather than cuts) the quadriceps muscle to access the joint. This muscle-sparing method helps preserve strength and can support faster post-operative recovery.
Once the joint is exposed, Dr Paterson evaluates the worn-out bone and cartilage and confirms alignment. Your patient-specific cutting guides are placed on your femur and tibia to guide precisely where bone needs to be removed. He may also use precision callipers to verify bone thickness, which supports kinematic alignment, ensuring the implant restores your natural joint height and angles.
Using the PSI cutting guides, Dr Paterson performs precise bone cuts that match your 3D surgical plan. This critical step helps:
- Preserve your natural joint motion
- Minimise disruption to surrounding tissues
- Achieve accurate, personalised implant positioning
Temporary trial components are inserted to check the movement, alignment, and balance of your new joint. Adjustments are made if needed to ensure smooth, stable motion and comfort before the final implants are secured.
Once the knee is optimally balanced, the final components are inserted:
- A metal femoral implant for the thigh bone
- A tibial baseplate and plastic insert for the shin bone
- A patellar button may be added if the underside of your kneecap is resurfaced
The components are secured with either bone cement or cementless fixation, based on your specific needs.
After your surgery, you’ll be taken to the recovery area where your vital signs will be closely monitored as the anaesthetic wears off. A nurse will keep you comfortable, and you’ll gradually regain full awareness.
Within the first few hours, most patients are moved from recovery to their hospital room. While you’ve had major surgery, it’s important to remember that you’re not “sick”, you’re recovering from a procedure that’s designed to improve your function, comfort, and mobility long term.
You’ll be encouraged to change back into your own clothes once you’re settled in your room. This small but meaningful step supports your independence, mobility, and sense of normalcy as you begin your recovery.
Most patients begin gentle movement and physiotherapy within 24 hours of surgery. Dr Paterson and his team will guide you through the early phases of recovery with a personalised, supportive plan that may include:
- Effective pain management to keep you comfortable and active
- Early mobilisation to reduce the risk of complications and improve recovery
- Use of crutches or walking aids, as needed, to help you move around safely
- Discharge planning and education on caring for your knee at home
From the very beginning, the focus is on helping you regain independence and get back to your daily life safely and confidently.
Your patient specific, kinematically aligned total knee replacement journey with Dr Darren Paterson: step by step
Undergoing a total knee replacement is a significant decision, and understanding the process can help you feel more confident and prepared. Dr Darren Paterson uses a highly personalised approach that combines Patient-Specific Instrumentation (PSI) and kinematic alignment, supported by the minimally invasive subvastus approach, to help restore your natural joint movement and improve long-term comfort. Here’s what you can expect from start to finish:
The surgical procedure
Your journey begins with a referral from your GP and an initial consultation with Dr Paterson. He will assess your knee’s alignment, stability, range of motion, and how your symptoms impact your everyday life. You’ll discuss whether total knee replacement is the most suitable option for your condition and what outcomes you can expect from surgery.
Once a decision is made to proceed, Dr Paterson will arrange for a CT scan of your entire leg. This scan provides detailed information about your bone structure and joint alignment, which is used to build a 3D model of your knee. This model forms the foundation of your customised surgical plan.
Using specialised planning software, Dr Paterson creates a precise surgical plan that maps out your implant positioning, sizing, and alignment based on your unique knee anatomy. This behind-the-scenes step typically takes 2–3 weeks and helps ensure the procedure is tailored to match your natural joint structure as closely as possible.
Before surgery, you’ll be provided with detailed instructions. This includes:
- Completing hospital admission paperwork
- Starting prehabilitation physiotherapy
- Booking your post-operative review appointments
- Preparing your home environment for recovery
Dr Paterson’s team will support you through each of these steps.
You’ll receive a pre-operative consultation with the anaesthesia team, usually by phone. Together, you’ll decide whether general anaesthesia or spinal anaesthesia is best for you, based on your medical history and preferences.
Before surgery, Dr Paterson will review the procedure with you, including the risks, benefits, and expected recovery. Once you’re confident and informed, you’ll sign a consent form. You’ll also receive advice on preparing your home and organising any support you may need after surgery.
Your 3D-printed cutting guides are manufactured in Switzerland, sterilised, and delivered to the hospital in time for your procedure. These instruments are uniquely designed to match your knee, ensuring the most accurate fit possible.
You’ll be admitted to hospital on the day of your surgery, usually a few hours before the scheduled procedure. The nursing and surgical team will prepare you and confirm that all pre-operative protocols are in place to ensure a smooth and safe operation.
Fasting Instructions
Your anaesthetist or hospital will provide specific instructions about fasting (not eating or drinking) before surgery. In most cases, you will be asked to:
- Stop eating at least 6 hours before your admission time
- Stop drinking clear fluids (e.g., water) 2 hours before surgery
It’s important to follow these instructions carefully to ensure your safety under anaesthesia. If you’re unsure about the timing, check with the hospital the day before.
What to Bring to Hospital
To help you feel comfortable and prepared, we recommend packing the following:
- Your hospital admission paperwork
- Any current medications in their original packaging
- Comfortable loose-fitting clothing for after surgery
- Slip-on shoes or supportive footwear (no laces)
- A list of any known allergies or medical conditions
- Personal items such as glasses, hearing aids, or dentures (if applicable)
- Your Medicare and private health insurance cards
- Mobile phone and charger (if desired)
Leave valuables and jewellery at home and remove any nail polish from your fingers and toes prior to arrival.
A nurse will help you change into your surgical gown and complete final checks. Once ready, you will be escorted to the operating theatre when it’s time for your procedure.
The surgical procedure
In the anaesthetic bay, you’ll meet your anaesthetist and receive your agreed anaesthetic. Once you are comfortable and asleep or sedated, your leg will be cleaned with antiseptic solution and sterile drapes will be placed around the knee. A tourniquet may be applied around your thigh to reduce bleeding and improve visibility during the procedure.
Dr Paterson will make a careful incision along the front of your knee. He uses the subvastus approach, a minimally invasive technique that gently lifts (rather than cuts) the quadriceps muscle to access the joint. This muscle-sparing method helps preserve strength and can support faster post-operative recovery.
Once the joint is exposed, Dr Paterson evaluates the worn-out bone and cartilage and confirms alignment. Your patient-specific cutting guides are placed on your femur and tibia to guide precisely where bone needs to be removed. He may also use precision callipers to verify bone thickness, which supports kinematic alignment, ensuring the implant restores your natural joint height and angles.
Using the PSI cutting guides, Dr Paterson performs precise bone cuts that match your 3D surgical plan. This critical step helps:
- Preserve your natural joint motion
- Minimise disruption to surrounding tissues
- Achieve accurate, personalised implant positioning
Temporary trial components are inserted to check the movement, alignment, and balance of your new joint. Adjustments are made if needed to ensure smooth, stable motion and comfort before the final implants are secured.
Once the knee is optimally balanced, the final components are inserted:
- A metal femoral implant for the thigh bone
- A tibial baseplate and plastic insert for the shin bone
- A patellar button may be added if the underside of your kneecap is resurfaced
The components are secured with either bone cement or cementless fixation, based on your specific needs.
After your surgery, you’ll be taken to the recovery area where your vital signs will be closely monitored as the anaesthetic wears off. A nurse will keep you comfortable, and you’ll gradually regain full awareness.
Within the first few hours, most patients are moved from recovery to their hospital room. While you’ve had major surgery, it’s important to remember that you’re not “sick”, you’re recovering from a procedure that’s designed to improve your function, comfort, and mobility long term.
You’ll be encouraged to change back into your own clothes once you’re settled in your room. This small but meaningful step supports your independence, mobility, and sense of normalcy as you begin your recovery.
Most patients begin gentle movement and physiotherapy within 24 hours of surgery. Dr Paterson and his team will guide you through the early phases of recovery with a personalised, supportive plan that may include:
- Effective pain management to keep you comfortable and active
- Early mobilisation to reduce the risk of complications and improve recovery
- Use of crutches or walking aids, as needed, to help you move around safely
- Discharge planning and education on caring for your knee at home
From the very beginning, the focus is on helping you regain independence and get back to your daily life safely and confidently.
Recovery timelines following a patient specific PSI), kinematically aligned total knee replacement
Recovery from total knee replacement surgery is a gradual process that occurs in stages, with most patients seeing steady progress over several months. When your procedure is performed using Patient-Specific Instrumentation (PSI) and the kinematic alignment technique, recovery may be smoother, as this approach aims to minimise soft tissue disruption and closely replicate your natural joint motion.
Below is a general timeline to help you understand what to expect at each stage of your recovery. Every patient is different, and your individual progress will depend on factors such as your age, overall health, and commitment to rehabilitation.
Day 0–1: Day of surgery and early recovery
- You’ll wake up in recovery where your vital signs will be monitored.
- Most patients are encouraged to stand and take a few steps (with assistance) within 24 hours of surgery.
- You’ll start gentle range-of-motion and leg exercises guided by your physiotherapist.
- Pain will be managed with medications and local anaesthetic, and you may be fitted with a knee brace or ice therapy device to reduce swelling.
Days 2–3: In-hospital rehabilitation
- You’ll continue working with your physiotherapy team on walking, stair climbing, and strengthening exercises.
- Most patients begin transitioning from a walker to crutches or walking sticks.
- Once you are able to safely walk short distances, manage stairs, and perform basic self-care tasks, you will be discharged home (usually on Day 2 or 3 post-op).
- You will be sent home with detailed recovery instructions and post-operative care guidelines.
Weeks 1–2: Home-based recovery begins
- Your focus will be on managing swelling and pain, gentle walking, and increasing your knee’s range of motion.
- You’ll continue prescribed exercises at home and may begin outpatient physiotherapy.
- You may be walking indoors with crutches or a cane, gradually increasing your independence.
- Many patients begin to wean off strong pain medications and transition to milder options as guided.
Weeks 3–6: Building strength and mobility
- You’ll likely notice significant improvements in your ability to walk and move more confidently.
- Crutches or walking aids may no longer be needed.
- Physiotherapy continues, focusing on improving flexibility, balance, and strengthening the muscles around the knee.
- You may start returning to light daily activities and some low-impact hobbies like gentle cycling or walking outdoors.
Weeks 6–12: Returning to routine activities
- Most patients return to part-time work or desk-based jobs around this time (depending on the nature of your work).
- You should be walking confidently without aids and climbing stairs more easily.
- Strengthening exercises will continue to support long-term joint stability and function.
- Driving may be possible again once you have regained full control of the operated leg (typically after 6 weeks if cleared by Dr Paterson).
3–6 months: Resuming everyday life
- Your knee should feel more stable, with greatly reduced pain and improved mobility.
- You may return to more active daily routines and recreational low-impact activities (e.g., swimming, golf, or long walks).
- Some patients resume full-time work and light physical jobs at this stage.
- Physiotherapy may taper off depending on your progress and goals.
6–12 months: Long-term results
- The majority of healing and functional gains occur in the first 12 months after surgery.
- Most patients report major improvements in pain, joint movement, and quality of life.
- The knee continues to remodel and strengthen, and activities like hiking or cycling may be more comfortable.
- High-impact activities like running or jumping should still be avoided to protect the joint and prolong implant life.
Monitoring your progress
You’ll have scheduled follow-up appointments with Dr Darren Paterson during your recovery. These appointments allow him to:
- Assess your wound healing and joint function
- Review your imaging and implant position (if needed)
- Adjust your recovery plan or address any concerns
A patient-specific, kinematically aligned total knee replacement offers a tailored approach to restoring comfort, mobility, and natural joint movement. By combining advanced 3D surgical planning, personalised instrumentation, and precise kinematic alignment, this technique aims to deliver a knee that feels more like your own, with less soft tissue disruption and a smoother recovery.
If knee pain is limiting your quality of life, and non-surgical treatments are no longer helping, a personalised knee replacement may be the next step forward.


